New BMJ Study: $14.2 Million Undisclosed Financial Conflicts in DSM-5-TR, the “Bible” of Psychiatry
Updated
Without question, unbiased, evidence-based mental health practices free from Big Pharma’s unethical influence are paramount to the health of our nation, especially now that the COVID-19 pandemic has pulled back the curtain on the anarchic corruption in American health care. In the United States and much of the world, the American Psychiatric Association’s (APA) Diagnostic and Statistical Manual of Mental Disorders (DSM) is the gold standard handbook for the diagnosis of mental disorders. To keep current, APA task force members recently revised the manual, which is now in its fifth edition and called DSM-5-TR (fifth text revision). In an effort to ensure the revisions were without industry influence, a recent investigation aimed to evaluate the financial ties the APA task force and panel members had with Big Pharma. And guess what? It turns out the “bible” of psychiatry, DSM-5-TR, included a whopping $14.2 million in undisclosed financial conflicts.
The special paper, titled “Undisclosed financial conflicts of interest in DSM-5-TR: cross-sectional analysis,” and published in the BMJ on January 10, 2024, explained that since 2013, under the Physician Payments Sunshine Act, all US drug and device manufacturers are required to disclose payments given to physicians and teaching hospitals. To facilitate this, the Centers for Medicare and Medicaid Services (CMS) developed the public access database called Open Payments, which identifies monies given by big pharma to individual physicians and institutions. As is undoubtedly the case with many drugs, including the deadly mRNA COVID-19 “vaccines,” the paper authors explained that Open Payments data can be used to determine the many ways financial conflicts of interest may influence physician behavior. The authors wrote:
“For example, this [Open Payments] database has been used to determine physicians’ likelihood to prescribe certain drugs and how that may have been influenced by compensation from the pharmaceutical industry.”
In their investigation, the study researchers found that 168 individuals were identified who served as either APA panel or task force members for revising the DSM-5-TR. Of that amount, 92 met the criteria of being a physician based in the US and, therefore, could be included in Open Payments. Six served on the task force, and 86 on the panel. When the study authors put their names in Open Payments, of the 92 individuals based in the US, 55 panel and task force members (53 panel and 2 task force members)—60 percent—had conflicts of interest (COI) during the selected timeframe of 2016-19. This period was chosen to include the year that development of the DSM-5-TR commenced and the three years preceding, a time consistent with previous research on conflicts of interest and consistent with the APA’s disclosure requirements for the fifth revision (DSM-5) of the manual.
Collectively, these 92 individuals received a total of $14.24 million. Wow, with that in mind, there is no telling how much bribe money from Big Pharma the members who are not in the US received. Incredibly, noting that the APA did not require that the DSM-5-TR disclose COI, the study quantified the extent and type of COIs received by panel and task-force members by manually entering each name into Open Payments. According to the study, when breaking down the $14.24 million, the most significant payment proportion, 70%, was for research funding, followed by 8.3% for consulting and 4.8% for travel. Oddly, research funding was excluded from the APA’s disclosure policy for DSM-5. Aware of the implications of omitting research funding, the study noted:
“Research funding was excluded from the American Psychiatric Association’s disclosure policy for DSM-5, and some individuals might believe that such compensation does not influence behavior. Nonetheless, evidence is lacking to suggest that simply because money comes in the form of a research grant it does not create an obligation to reciprocate or invoke an implicit bias.”
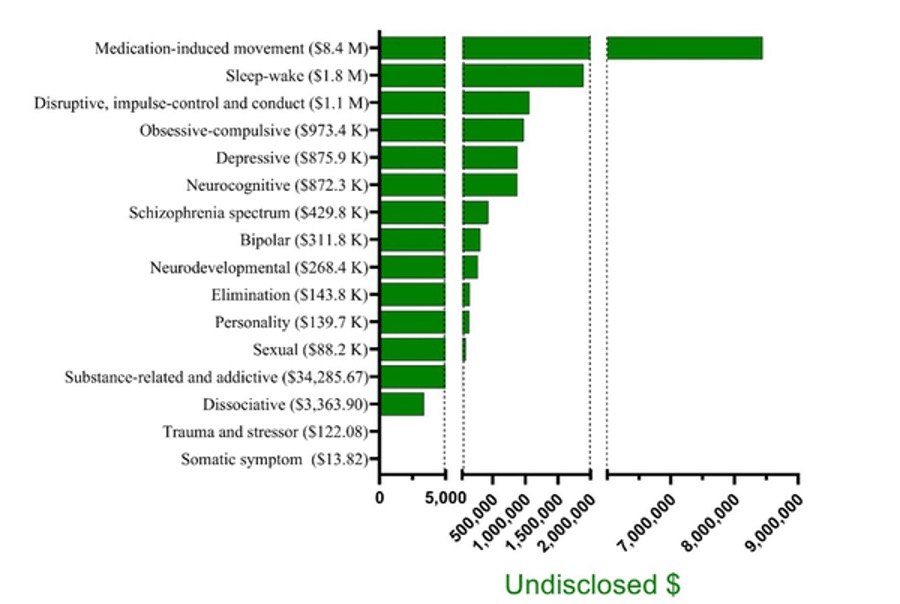
Further examination of the workgroups revealed significant differences in undisclosed compensation. Although anxiety disorders, feeding and eating disorders, gender dysphoria, and paraphilic disorder work group members received no compensation, the amount received by other workgroups was considerable:
Obsessive-compulsive disorders = $973,851
Disruptive disorders = $1,059,910
Sleep-week disorders = $1,892,431
Medication-induced movement disorders = $8,443,468
Study author Lauren C. Davis, MBS, remarked that the findings likely underestimate monies received because 45% of working group members include PhDs and others who are not tracked in Open Payments. Nonetheless, the study backs up what literally all studies that have evaluated the association between industry payments and physician prescribing have concluded—that industry payments were associated with increased subscribing of the paying company’s drug, increased prescribing costs, and increased prescribing of branded drugs. After all, that is how bribery works. With that in mind, Americans concerned about COIs by their healthcare providers should immediately become familiar with Open Payments. Look them up, see who’s paying them, and pay attention to a connection in their treatment plan.
With mental health exceptionally vulnerable during and following the pandemic, and considering that the DSM is known as the “bible” of psychiatry, $14.2 million in undisclosed industry compensation from pharmaceutical companies to the DSM-5-TR developers is unacceptable and a severe cause for concern. Davis remarked that “industry influence over the development of this diagnostic guideline can have a profound effect on public health (e.g., by broadening diagnostic categories and influencing what medications will be prescribed and covered by insurance).”
She’s exactly right. Thus, thanks to Davis and the other researchers behind the study, an obvious question arises: why didn’t the APA—which, by the way, does not publicly disclose minutes of the meetings of Diagnostic and Statistical Manual of Mental Disorders, nor does it provide descriptive summaries of proposed changes and reasons for inclusion or exclusion of the proposed changes—make it mandatory that its task force and panel members fully disclose what Big Pharma entities are pulling their strings? Before the next crisis, which society has been assured of, the diagnosis and treatment of mental health issues must be free of industry influence or even the appearance of such influence. Speaking of the conflicts, Davis remarked:
“There is an abundance of research documenting the impact of financial conflicts of interest on medical literature, including randomized clinical trials, meta-analyses, and clinical diagnostic and practice guidelines. Such research has consistently shown that conflicts of interest lead to subtle but impactful pro-industry thinking and conclusions.”
Big Pharma’s influence on the APA’s DSM-5-TR gold-standard manual (and previous versions) is unacceptable. Yet, unfortunately, similar to the corruptible actions of the American Heart Association (AMA) as heart attacks rise in young people, the APA receives funding from Big Pharma through its American Psychiatric Association Foundation (APAF). Sigh. With Big Pharma lining its pockets, it stands to reason that when the APA issued a press release last November titled “Stress in America 2023, A nation recovering from trauma,” a red flag should immediately be raised. Indeed.
Following the deep-stated funded freedom-robbing, health-destroying script of the World Health Organization and others like it, the APA reported that “there is mounting evidence that our society is experiencing the psychological impacts of a collective trauma” following the COVID-19 pandemic. The press release explained that “global conflict, racism and racial injustice, inflation, and climate-related disasters are all weighing on the collective consciousness of Americans.” But alas, never fear. They’ve teamed up with Big Pharma to pay American physicians to diagnose and prescribe drugs to treat mental illness that, given the corrupt state of affairs, have no trustworthy safety or efficacy data. And, to succeed, they’re banking on the fact people don’t catch on. But thanks to people like Davis and so many others, they are. Remarking that the “aftermath” of the pandemic remains a traumatic experience among most Americans, Arthur C. Evans Jr., Ph.D., APA’s chief executive officer, stated:
“We cannot ignore the fact that we have been significantly changed by the loss of more than one million Americans, as well as the shift in our workplaces, school systems, and culture at large. To move toward posttraumatic growth, we must first identify and understand the psychological wounds that remain.”